Volume 115, Nº 1, July 2020
DOI: https://doi.org/10.36660/abc.20190393
ORIGINAL ARTICLE
Implementation of a Best Practice in Cardiology (BPC) Program Adapted from Get With The Guidelines® in Brazilian Public Hospitals: Study Design and Rationale
Fabio Papa Taniguchi
Sabrina Bernardez-Pereira
Suzana Alves Silva
Antônio Luiz Pinho Ribeiro
Louise Morgan
Anne B. Curtis
Kathryn Taubert
Denilson Campos de Albuquerque
Bernadete Weber
Pedro Paulo Magalhães Chrispim
Camila Pereira Pinto Toth
Erica Deji Moura Morosov
Gregg C. Fonarow
Sidney C. Smith Jr.
Angelo Amato Vincenzo de Paola
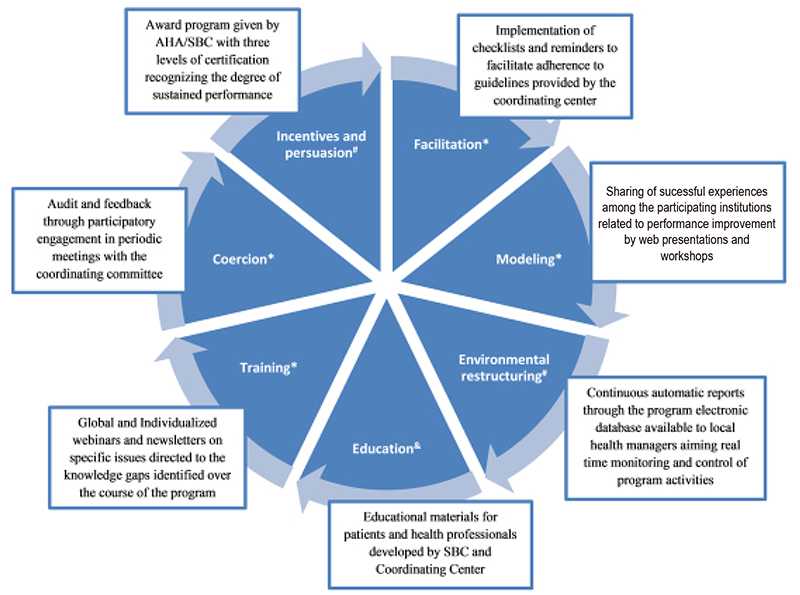
Figure 1 – Intervention axes *Target of behavior change: health professionals &Target of behavior change: Patients and health professionals # Target of behavior change: Health managers.
Abstract
Background: There are substantial opportunities to improve the quality of cardiovascular care in developing countries through the implementation of a quality program.
Objective: To evaluate the effect of a Best Practice in Cardiology (BPC) program on performance measures and patient outcomes related to heart failure, atrial fibrillation and acute coronary syndromes in a subset of Brazilian public hospitals.
Methods: The Boas Práticas em Cardiologia (BPC) program was adapted from the American Heart Association’s (AHA) Get With The Guidelines (GWTG) Program for use in Brazil. The program is being started simultaneously in three care domains (acute coronary syndrome, atrial fibrillation and heart failure), which is an approach that has never been tested within the GWTG. There are six axes of interventions borrowed from knowledge translation literature that will address local barriers identified through structured interviews and regular audit and feedback meetings. The intervention is planned to include at least 10 hospitals and 1,500 patients per heart condition. The primary endpoint includes the rates of overall adherence to care measures recommended by the guidelines. Secondary endpoints include the effect of the program on length of stay, overall and specific mortality, readmission rates, quality of life, patients’ health perception and patients’ adherence to prescribed interventions.
Results: It is expected that participating hospitals will improve and sustain their overall adherence rates to evidence based recommendations and patient outcomes. This is the first such cardiovascular quality improvement (QI) program in South America and will provide important information on how successful programs from developed countries like the United States can be adapted to meet the needs of countries with developing economies like Brazil. Also, a successful program will give valuable information for the development of QI programs in other developing countries.
Conclusions: This real-world study provides information for assessing and increasing adherence to cardiology guidelines in Brazil, as well as improvements in care processes. (Arq Bras Cardiol. 2020; 115(1):92-99).
Keywords: Cardiovascular Diseases/physiopathology; Heart Failure; Atrial Fibrillation; Acute Coronary Syndrome; Quality Improvement/trends; Guidelines as Topic.