Volume 110, Nº 2, February 2018
DOI: http://www.dx.doi.org/10.5935/abc.20180023
ORIGINAL ARTICLE
Current Practices in Myocardial Perfusion Scintigraphy in Brazil and Adherence to the IAEA Recommendations: Results of a Cross Sectional Study
Carlos Vitor Braga Rodrigues
Anderson Oliveira
Christiane Cigagna Wiefels
Maurício de Souza Leão
Cláudio Tinoco Mesquita
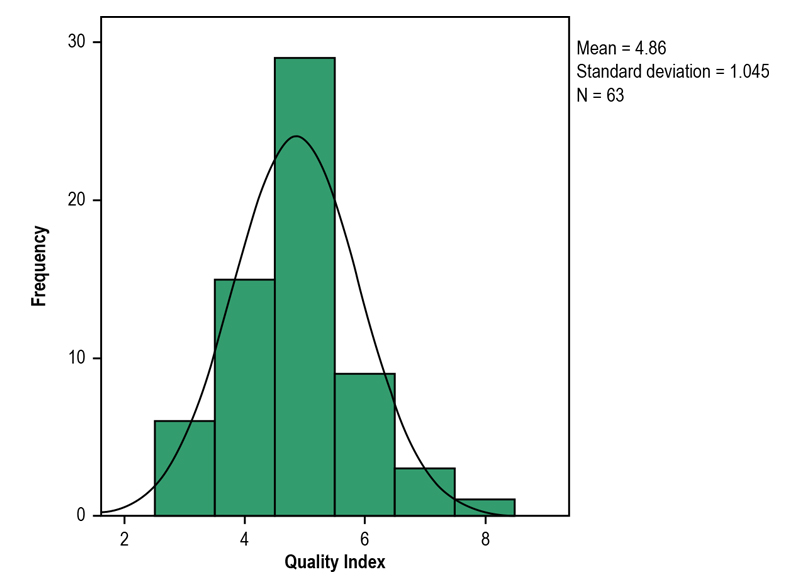
Figure 1 – Distribution of the quality index (0 to 8) of good practices of 63 nuclear cardiology services in Brazil, 2016.
Abstract
Background: Data on the current situation of nuclear medicine practices in cardiology in Brazil are scarce. The International Atomic Energy Agency (IAEA) has recommended eight “good practices” to minimize patients’ ionizing radiation exposure during myocardial perfusion scintigraphy (MPS).
Objectives: To assess the adoption of the eight good practices in MPS in Brazil. Methods: Cross-sectional study with data obtained by use of a questionnaire. All hypothesis tests performed considered a significance level of 5%.
Results: We observed that 100% of the nuclear medicine services (NMS) assessed do not use thallium-201 as the preferred protocol. Regarding the use of technetium-99m, 57% of the NMS administer activities above the threshold recommended by the IAEA (36 mCi) or achieve an effective dose greater than 15 millisievert (mSv). The abbreviated stress-only myocardial perfusion imaging is not employed by 94% of the NMS; thus, only 19% count on strategies to reduce the radioactive doses. Approximately 52% of the NMS reported always performing dose adjustment for patient’s weight, while 35% administer poorly calculated doses in the one-day protocol.
Conclusion: A considerable number of NMS in Brazil have not adopted at least six practices recommended by the IAEA. Despite the difficulties found in nuclear practice in some Brazilian regions, almost all obstacles observed can be overcome with no cost increase, emphasizing the importance of developing strategies for adopting “good practices” when performing MPS. (Arq Bras Cardiol. 2018; 110(2):175-180)
Keywords: Nuclear Medicine / methods; Myocardial Perfusion Imaging; Myocardial Ischemia / diagnostic imaging.