Volume 114, Nº 4, April 2020
DOI: https://doi.org/10.36660/abc.20190736
ORIGINAL ARTICLE
Analysis of >100,000 Cardiovascular Surgeries Performed at the Heart Institute and a New Era of Outcomes
Omar A.V. Mejia
Luiz Augusto Ferreira Lisboa
Luiz Fernando Caneo
Elisandra Trevisan Arita
Carlos Manuel de Almeida Brandão
Ricardo Ribeiro Dias
Roberto Costa
Marcelo Biscegli Jatene
Pablo Maria Alberto Pomerantzeff
Luís Alberto Oliveira Dallan
Fabio Biscegli Jatene
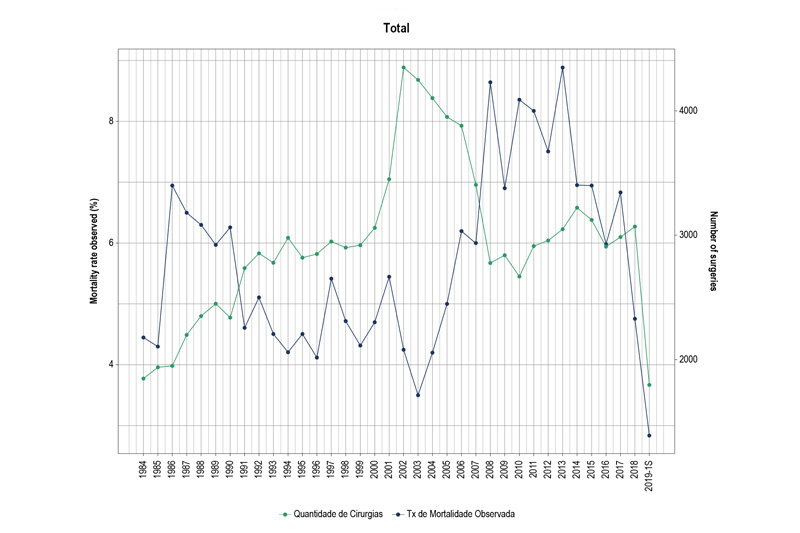
Figure 1 – Year-by-year graph of global surgical volume and mortality in > 35 years of the InCor.
Abstract
Background: The current challenge of cardiovascular surgery (CVS) is to improve the outcomes in increasingly severe patients. In this respect, continuous quality improvement (CQI) programs have had an impact on outcomes.
Objective: To assess the evolution of the incidence and mortality due to CVS, as well as the current outcomes of the Hospital das Clínicas Heart Institute of the University of São Paulo Medical School (InCor-HCFMUSP).
Methods: An outcome analysis of CVSs performed at the InCor, between January 1984 and June 2019. We observed the surgical volume and mortality rates in 5 time periods: 1st (1984-1989), 2nd (1990-1999), 3rd (2000-2007), 4th (2008-2015) and 5th (2016-2019). The CQI program was implemented between 2015 and 2016. The analysis included the total number of surgeries and the evolution of the most frequent procedures.
Results: A total of 105,599 CCVs were performed, with an annual mean of 2,964 procedures and mortality of 5,63%. When comparing the 4th and the 5th periods, the average global volume of surgeries was increased from 2,943 to 3,139 (p = 0.368), bypass graft (CABG), from 638 to 597 (p = 0.214), heart valve surgery, from 372 to 465 (p = 0.201), and congenital heart disease surgery, from 530 to 615 (p = 0.125). The average global mortality went from 7.8% to 5% (p < 0.0001); in CABG surgery, from 5.8% to 3.1% (p < 0.0001); in heart valve surgery, from 14% to 7.5% (p < 0.0001) and in congenital heart disease surgery, from 12.1% to 9.6% (p < 0.0001).
Conclusion: In spite of a recent trend towards increased surgical volume, there was a significant decrease in operative mortality in the groups studied. After the implementation of the CQI program, the mortality rates were closer to international standards. (Arq Bras Cardiol. 2020; 114(4):603-612)
Keywords: Cardiovascular Surgical Procedures/trends; Quality Improvement; Patient Safety; Hospital Mortality; Database.