Volume 114, Nº 3, March 2020
DOI: https://doi.org/10.36660/abc.20180076
ORIGINAL ARTICLE
Anticoagulation Therapy in Patients with Non-valvular Atrial Fibrillation in a Private Setting in Brazil: A Real‑World Study
Pedro Gabriel Melo de Barros e Silva
Henry Sznejder
Rafael Vasconcellos
Georgette M. Charles
Hugo Tannus F. Mendonca-Filho
Jack Mardekian
Rodrigo Nascimento
Stephen Dukacz
Manuela Di Fusco
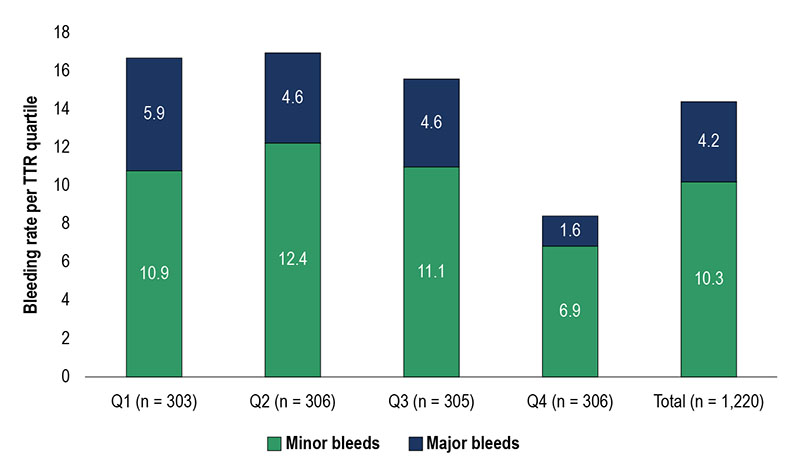
Figure 3 – Bleeding rate per TTR quartile.
Abstract
Background: The safety and effectiveness of warfarin depend on anticoagulation control quality. Observational studies associate poor control with increased morbidity, mortality and healthcare costs.
Objectives: To develop a profile of non-valvular atrial fibrillation (NVAF) patients treated with warfarin in a Brazilian private ambulatory and hospital setting, evaluate the quality of anticoagulation control, and its association with clinical and economic outcomes.
Methods: This retrospective study, through a private health insurance dataset in Brazil, identified NVAF patients treated with warfarin between 01 MAY 2014 to 30 APRIL 2016, described their anticoagulation management, and quantified disease-related costs. Data on demographics, clinical history, concomitant medication and time in therapeutic range (TTR) of international normalized ratio (INR) values were retrieved. Patients were grouped into TTR quartiles, with good control defined as TTR ≥ 65% (Rosendaal method). Major bleeds and all-cause direct medical costs were calculated and compared between good and poor control subgroups. P-values < 0.05 were considered statistically significant.
Results: The analysis included 1220 patients (median follow-up: 1.5 years; IQR: 0.5–2.0). On average, each patient received 0.95 monthly INR measurements (mean INR: 2.60 ± 0.88, with 26.1% of values < 2 and 24.8% > 3), (median TTR: 58%; IQR: 47–68%), (mean TTR: 56.6% ± 18.9%). Only 31% of patients were well-controlled (mean TTR: 78% ± 10%), with 1.6% having major bleeds within median follow‑up, and direct medical costs per member per year (PMPY) of R$25,352(± R$ 37,762). Poorly controlled patients (69%) were associated with 3.3 times more major bleeds (5.3% vs. 1.6%; p < 0.01) and 40% higher costs (R$35,384 vs. R$25,352; p < 0.01).
Conclusions: More than 60% of the patients were below the desired target and the associated costs were higher. (Arq Bras Cardiol. 2020; 114(3):457-466)
Keywords: Warfarine/therapeutic use; Anticoagulants/adverse effects; Atrial Fibrillation/comlications; Hospitals, Private/ economics; Health Care Quality, Access and Evaluation.