Volume 114, Nº 2, February 2020
DOI: http://www.dx.doi.org/10.5935/abc.10.5935/abc.20190193
ORIGINAL ARTICLE
Longitudinal Shortening of the Left Ventricle by Cine-CMR for Assessment of Diastolic Function in Patients with Aortic Valve Disease
Sergio Marrone Ribeiro
Clerio Francisco de Azevedo Filho
Roney Sampaio
Flávio Tarasoutchi
Max Grinberg
Roberto Kalil-Filho
Carlos Eduardo Rochitte
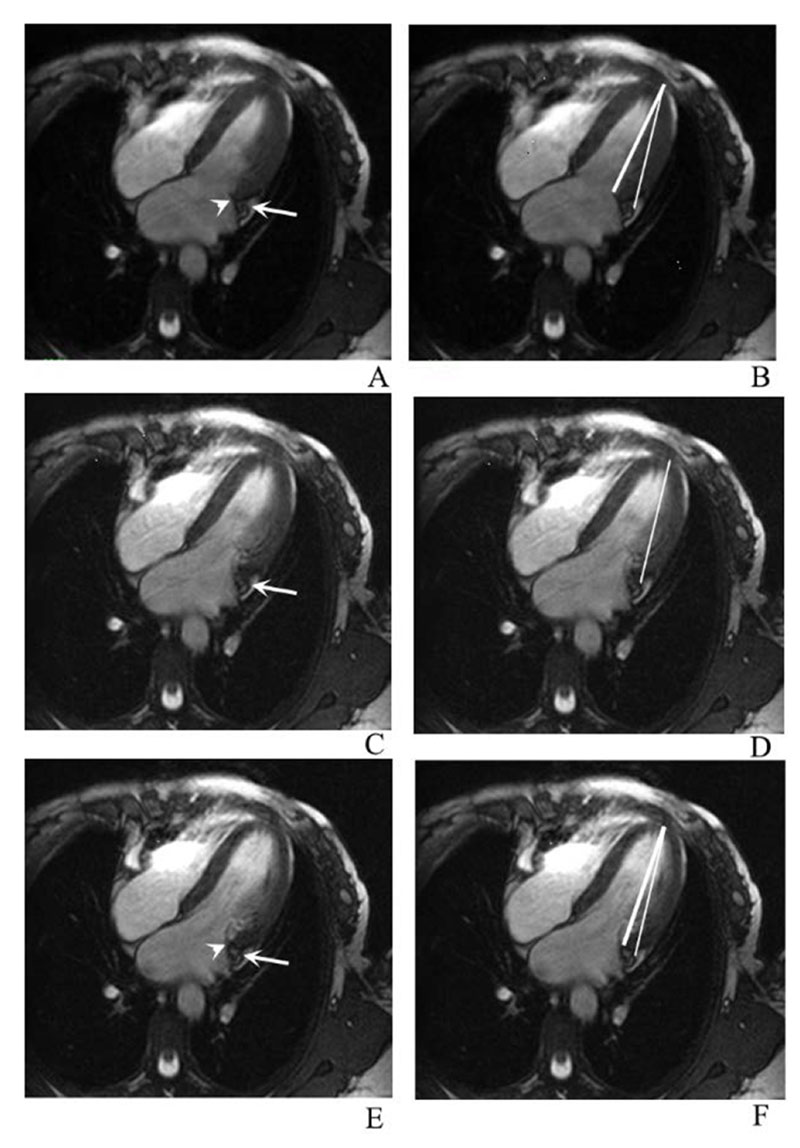
Figure 1 – Longitudinal displacement of the atrioventricular junction (AVJ). The same four- chamber slice is shown in three different cardiac phases during AVJ rapid movement: A and B, C and D, E and F. On the left column the arrowhead represents the reference used by Saba et al.9 and the thin arrow shows the anatomical reference used in the present study. Note that when the cardiac motion is faster (small arrow in C and D), we could not precisely identify the site of the mitral valve insertion; however, the adjacent coronary sinus wall is still well defined. On the right column, we showed the lines used for the LV longitudinal measurements on this study (thinner line) and by Saba et al.9 (thicker line) .
Abstract
Background: Diastolic dysfunction, commonly evaluated by echocardiography, is an important early finding in many cardiomyopathies. Cardiac magnetic resonance (CMR) often requires specialized sequences that extends the test time. Recently, feature-tracking imaging has been made available, but still requires expensive software and lacks clinical validation.
Objective: To assess diastolic function in patients with aortic valve disease (AVD) and compare it with normal controls by evaluating left ventricular (LV) longitudinal displacement by CMR.
Methods: We compared 26 AVD patients with 19 normal controls. Diastolic function was evaluated as LV longitudinal displacement in 4-chamber view cine-CMR images using steady state free precession (SSFP) sequence during the entire cardiac cycle with temporal resolution < 50 ms. The resulting plot of atrioventricular junction (AVJ) position versus time generated variables of AVJ motion. Significance level of p < 0.05 was used.
Results: Maximum longitudinal displacement (0.12 vs. 0.17 cm), maximum velocity during early diastole (MVED, 0.6 vs. 1.4s-1), slope of the best-fit line of displacement in diastasis (VDS, 0.22 vs. 0.03s-1), and VDS/MVED ratio (0.35 vs. 0.02) were significantly reduced in AVD patients compared with controls, respectively. Aortic regurgitation showed significantly worse longitudinal LV shortening compared with aortic stenosis. Higher LV mass indicated worse diastolic dysfunction.
Conclusions: A simple linear measurement detected significant differences on LV diastolic function between AVD patients and controls. LV mass was the only independent predictor of diastolic dysfunction in these patients. This method can help in the evaluation of diastolic dysfunction, improving cardiomyopathy detection by CMR, without prolonging exam time or depending on expensive software. (Arq Bras Cardiol. 2020; 114(2):284-292)
Keywords: Cardiovascular Diseases/mortality; Cardiomyopathy, Hypertrophic/complications; Diagnostic Imaging; Echocardiography; Magnetic Resonance Spectroscopy; Heart Failure; Aortic Valve Insufficiency.