Volume 111, Nº 6, December 2018
DOI: http://www.dx.doi.org/10.5935/abc.20180199
ORIGINAL ARTICLE
The Prognostic Value and Clinical Use of Myocardial Perfusion Scintigraphy in Asymptomatic Patients after Percutaneous Coronary Intervention
Larissa Franco de Andrade
Ana Carolina Souza
Thais Peclat
Caio Bartholo
Thalita Pavanelo
Ronaldo de Souza Leão Lima
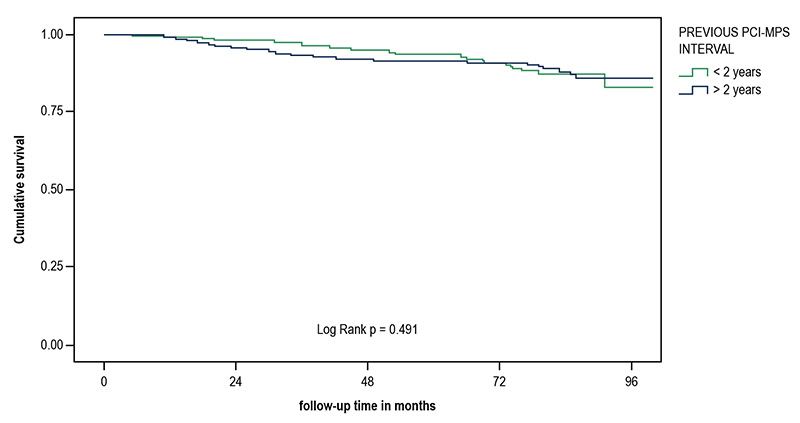
Figure 3 – Kaplan-Meier survival curve of mortality according to previous PCI-MPS interval shorter or longer than 2 years.
Abstract
Background: The role of myocardial perfusion scintigraphy (MPS) in the follow-up of asymptomatic patients after percutaneous coronary intervention (PCI) is not established.
Objectives: To evaluate the prognostic value and clinical use of MPS in asymptomatic patients after PCI.
Methods: Patients who underwent MPS consecutively between 2008 and 2012 after PCI were selected. The MPS were classified as normal and abnormal, the perfusion scores, summed stress score (SSS), and summed difference score (SDS) were calculated and converted into percentage of total perfusion defect and ischemic defect. The follow-up was undertaken through telephone interviews and consultation with the Mortality Information System. Primary endpoints were death, cardiovascular death, and nonfatal acute myocardial infarction (AMI), and secondary endpoint was revascularization. Logistic regression and COX method were used to identify the predictors of events, and the value of p < 0.05 was considered statistically significant.
Results: A total of 647 patients were followed for 5.2 ± 1.6 years. 47% of MPS were normal, 30% were abnormal with ischemia, and 23% were abnormal without ischemia. There were 61 deaths, 27 being cardiovascular, 19 non fatal AMI, and 139 revascularizations. The annual death rate was higher in those with abnormal perfusion without ischemia compared to the groups with ischemia and normal perfusion (3.3% × 2% × 1.2%, p = 0.021). The annual revascularization rate was 10.3% in the ischemia group, 3.7% in those with normal MPS, and 3% in those with abnormal MPS without ischemia. The independent predictors of mortality and revascularization were, respectively, total perfusion defect greater than 6%, and ischemic defect greater than 3%. Forty-two percent of the patients underwent MPS less than 2 years after PCI, and no significant differences were observed in relation to those who underwent it after that period.
Conclusion: Although this information is not contemplated in guidelines, in this study MPS was able to predict events in asymptomatic after PCI patients, regardless of when they were performed. (Arq Bras Cardiol. 2018; 111(6):784-793)
Keywords: Myocardial Infarction; Coronary Artery Disease; Myocardial Revascularization; Heart/diagnostic imaging; Percutaneous Coronary Intervention.