Volume 110, Nº 3, March 2018
DOI: http://www.dx.doi.org/10.5935/abc.20180052
ARTIGO ORIGINAL
Echocardiographic Assessment of Ventricular Function in Young Patients with Asthma
Camilla Rayane De-Paula
Giselle Santos Magalhães
Nulma Souto Jentzsch
Camila Figueredo Botelho
Cleonice de Carvalho Coelho Mota
Tatiane Moisés Murça
Lidiana Fatima Correa Ramalho
Timothy C. Tan
Carolina Andrade Braganca Capuruço
Maria da Gloria Rodrigues-Machado
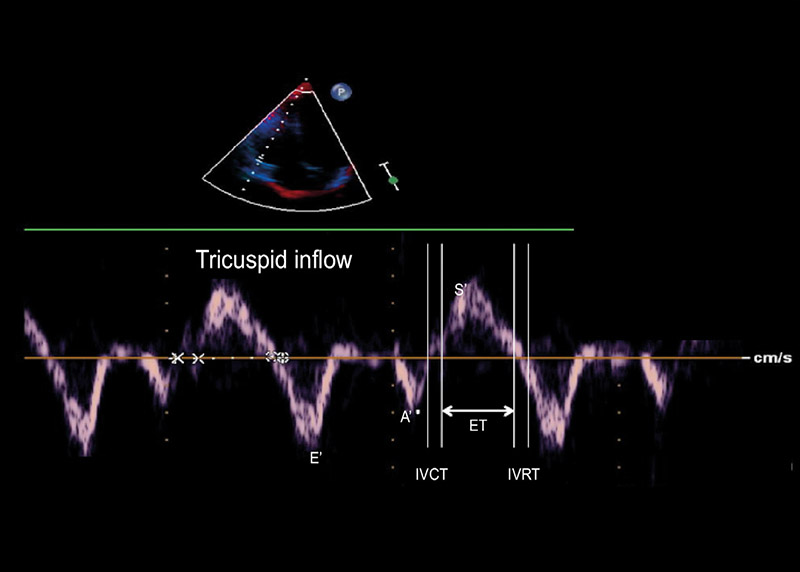
Figure 1 – Tissue Doppler imaging performed at tricuspid annulus in apical 4-chamber view (E’- peak early diastolic annular tricuspid velocity; A’: peak late diastolic annular tricuspid velocity; S´: systolic annular velocity; IVRT: isovolumetric relaxation time; IVCT: isovolumetric contraction time; ET: ejection time).
Abstract
Background: Despite significant advances in understanding the pathophysiology and management of asthma, some of systemic effects of asthma are still not well defined.
Objectives: To compare heart function, baseline physical activity level, and functional exercise capacity in young patients with mild-to-moderate asthma and healthy controls.
Methods: Eighteen healthy (12.67 ± 0.39 years) and 20 asthmatics (12.0 ± 0.38 years) patients were enrolled in the study. Echocardiography parameters were evaluated using conventional and tissue Doppler imaging (TDI).
Results: Although pulmonary acceleration time (PAT) and pulmonary artery systolic pressure (PASP) were within normal limits, these parameters differed significantly between the control and asthmatic groups. PAT was lower (p < 0.0001) and PASP (p < 0.0002) was higher in the asthma group (114.3 ± 3.70 ms and 25.40 ± 0.54 mmHg) than the control group (135.30 ± 2.28 ms and 22.22 ± 0.40 mmHg). The asthmatic group had significantly lower early diastolic myocardial velocity (E’, p = 0.0047) and lower E’ to late (E’/A’, p = 0.0017) (13.75 ± 0.53 cm/s and 1.70 ± 0.09, respectively) compared with control group (15.71 ± 0.34 cm/s and 2.12 ± 0.08, respectively) at tricuspid valve. In the lateral mitral valve tissue Doppler, the asthmatic group had lower E’ compared with control group (p = 0.0466; 13.27 ± 0.43 cm/s and 14.32 ± 0.25 cm/s, respectively), but there was no statistic difference in the E’/A’ ratio (p = 0.1161). Right isovolumetric relaxation time was higher (p = 0.0007) in asthmatic (57.15 ± 0.97 ms) than the control group (52.28 ± 0.87 ms), reflecting global myocardial dysfunction. The right and left myocardial performance indexes were significantly higher in the asthmatic (0.43 ± 0.01 and 0.37 ± 0.01, respectively) compared with control group (0.40 ± 0.01 and 0.34 ± 0.01, respectively) (p = 0.0383 and p = 0.0059, respectively). Physical activity level, and distance travelled on the six-minute walk test were similar in both groups.
Conclusion: Changes in echocardiographic parameters, evaluated by conventional and TDI, were observed in mild-to-moderate asthma patients even with normal functional exercise capacity and baseline physical activity level. Our results suggest that the echocardiogram may be useful for the early detection and evoluation of asthma-induced cardiac changes. (Arq Bras Cardiol. 2018; 110(3):231-239)
Keywords: Exertional Dyspnea / physiopathology; Echocardiography, Doppler; Asthma / physiopathology; Vascular Remodeling, Ventricular Dysfunction.