Volume 115, Nº 2, August 2020
DOI: https://doi.org/10.36660/abc.20190161
ORIGINAL ARTICLE
Discrepancy between International Guidelines on the Criteria for Primary Prevention of Sudden Cardiac Death in Hypertrophic Cardiomyopathy
Beatriz Piva e Mattos
Fernando Luís Scolari
Henrique Iahnke Garbin
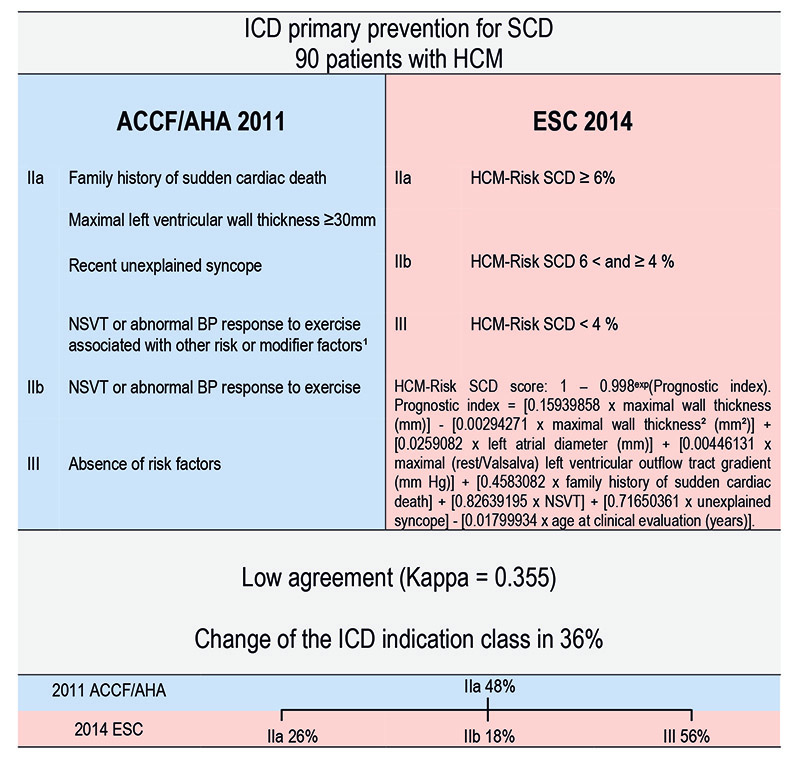
Figure 1 – Discrepancy between the 2011 ACCF/AHA and the 2014 ESC guidelines on sudden cardiac death primary pr evention in hypertrophic cardiomyopathy ICD = implantable cardioverter defibrillator, SCD = sudden cardiac death, HCM = hypertrophic cardiomyopathy, ACCF= American College of Cardiology Foundation, AHA = American Heart Association, ESC = European Society of Cardiology, NSVT = non-sustained ventricular tachycardia, BP = blood pressure; ¹Modifier factors: 1. Left ventricular outflow tract gradient ≥30 mmHg; 2. Late gadolineum enhancement on cardiac magnetic resonance; 3.Left ventricular apical aneurysm; 4. Malignant genetic mutation..
Abstract
Background: Risk stratification for sudden cardiac death (SCD) in hypertrophic cardiomyopathy (HCM) is based on different algorithms proposed by the 2011 ACCF/AHA and 2014 ESC guidelines.
Objective: To analyze the 2014 ESC model for SCD risk stratification and primary prevention ICD (implantable cardioverter defibrillator) in HCM in comparison to the North American guideline.
Methods: An HCM cohort was evaluated and the ESC HCM-Risk SCD score was calculated. Agreement of ICD recommendations criteria between the two guidelines was analyzed with Kappa coefficient. P<0.05 was adopted for the statistical analysis.
Results: In 90 consecutive patients followed for 6±3 years, the mean calculated ESC risk score was 3.2±2.5%. The risk predictors that have mainly contributed to the score calculation in the low (1.88% [1.42–2.67]), intermediate (5.17% [4.89–5.70]) and high-risk (7.82% [7.06–9.19]) categories were: maximal left ventricular wall thickness (1.60% [1.25–2.02]; 3.20% [3.18–3.36]; 4.46% [4.07–5.09]), left atrial diameter (0.97% [0.83–1.21]; 1.86% [1.67 2.40]; 2.48% [2.21–3.51]) and age (-0.91% [0.8–1.13]; -1.90% [1.12–2.03]; -2.34% [1.49–2.73]). The European model decreased the ICD recommendations in 32 (36%) patients. Among the 43 (48%) individuals with class IIa recommendation under the 2011 ACCF/AHA guideline, 8 (18%) were downgraded to class IIb and 24 (56%) to class III. Low agreement was found between the two systems: Kappa=0.355 and p=0.0001. In 8 (9%) patients with SCD or appropriate shock, 4 (50%) met class IIa indication with the 2011 ACCF/AHA guideline, but none achieved this class of recommendation with the 2014 ESC model.
Conclusion: Low agreement was found between the two strategies. The novel ESC model decreased the ICD recommendations, especially in those with class IIa recommendation, but left unprotected all patients with SCD or appropriate shock. (Arq Bras Cardiol. 2020; 115(2):197-204)
Keywords: Cardiomyopathy,Hypertrophic/genetics; Heredity; Death,Sudden, Cardiac; Arrhythmias, Cardiac; Syncope; Defibrillators,Implantable; Cohort Studies.