Volume 115, Nº 1, July 2020
DOI: https://doi.org/10.36660/abc.20180292
ORIGINAL ARTICLE
Cost-effectiveness of Drug-Eluting Stents in Percutaneous Coronary Intervention in Brazil’s Unified Public Health System (SUS)
João Addison Pessoa
Edirley Maia
Felipe Maia
Maurício Salles de Oliveira
Denizar Viana Araújo
Esmeralci Ferreira
Denilson Campos de Albuquerque
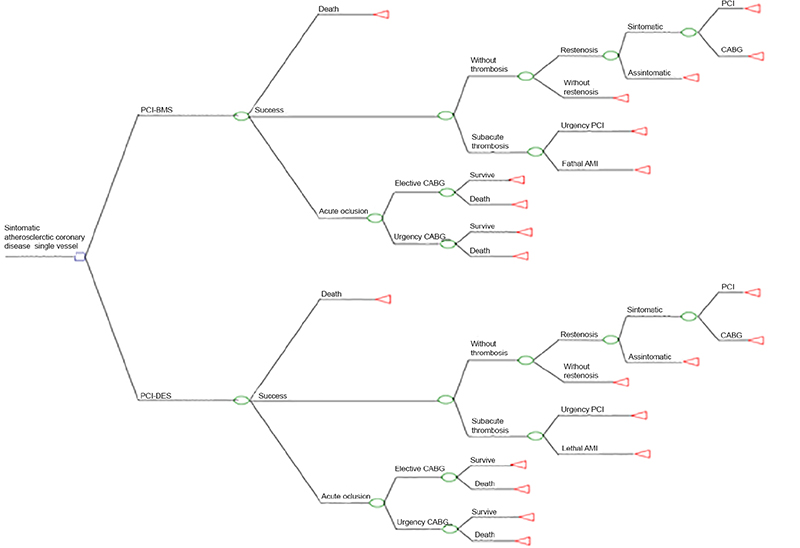
Figure 1 – CABG: coronary artery by-pass graft; PCI-BMS: percutaneous coronary intervention witn bare metal stent; PCI-DES: percutaneous coronary intervention with drug elution stent. Source: Polanczyk et al(2007)3
Abstract
Background: The use of drug-eluting stents (DESs), compared with bare-metal stents (BMSs), in percutaneous coronary intervention (PCI) has reduced the rate of restenosis, without an impact on mortality but with an increase in costs. Medical literature lacks randomized studies that economically compare these 2 stent types within the reality of the Brazilian Unified Public Health System (SUS).
Objective: To estimate the incremental cost-effectiveness ratio (ICER) between DES and BMS in SUS patients with singlevessel coronary artery disease.
Methods: Over a 3-year period, patients with symptomatic single-vessel coronary artery disease were randomized in a 1:2 ratio to receive a DES or BMS during PCI, with a 1-year clinical follow-up. The evaluation included instent restenosis (ISR), target lesion revascularization (TLR), major adverse events, and cost-effectiveness for each group. P-values <0.05 were considered significant.
Results: In the DES group, of 74 patients (96.1%) who completed the follow-up, 1 developed ISR (1.4%), 1 had TLR (1.4%), and 1 died (1.4%), with no cases of thrombosis. In the BMS group, of 141 patients (91.5%), ISR occurred in 14 (10.1%), TLR in 10 (7.3%), death in 3 (2.1%), and thrombosis in 1 (0.74%). In the economic analysis, the cost of the procedure was R$ 5,722.21 in the DES group and R$ 4,085.21 in the BMS group. The effectiveness by ISR and TLR was 8.7% for DES and 5.9% for BMS, with an ICER of R$ 18,816.09 and R$ 27,745.76, respectively.
Conclusions: In the SUS, DESs were cost-effective in accordance with the cost-effectiveness threshold recommended by the World Health Organization (Arq Bras Cardiol. 2020; 115(1):80-89)
Keywords: Myocardial Infarction; Percutaneous Coronary Intervention; Drug-Eluting Stents; Coronary Reestenosis; Cost-Benefit Analysis; Unified Health System (SUS).