Volume 114, Nº 6, June 2020
DOI: https://doi.org/10.36660/abc.20200096
ORIGINAL ARTICLE
Catheter Ablation for Treatment of Atrial Fibrillation and Supraventricular Arrhythmias Without Fluoroscopy Use: Acute Efficacy and Safety
Eduardo B. Saad
Charles Slater
Luiz Antonio Oliveira Inácio Jr.
Gustavo Vignoli dos Santos
Lucas Carvalho Dias
Luiz Eduardo Montenegro Camanho
video 1 - Catheter insertion from the femoral access to the RA guided by the electroanatomic mapping system. After the catheters arrive in the RA (decapolar catheter followed by the ablation catheter [RF]), marked by the appearance of electrograms, the RA anatomy is created, followed by cannulation of the coronary sinus (CS) – first by the RF catheter and followed by the decapolar one.
video 2 - Zero-fluoro transseptal puncture. After the ICE catheter is positioned in the RA, the LA and SVC are visualized. The guidewire arrives in the SVC, followed by sheath advancement. Sheath position in the SVC is confirmed by saline injection, showing craniocaudal flow. Septal tenting and perforation are shown, followed by wire advancement to the left PV. The sheath is then confirmed in the LA cavity by saline bubble visualization. The second transseptal sheath is then pulled down from the SVC to the septum, followed by a second septal perforation.
video 3 - High definition anatomic reconstruction of LA and PVs. With the multipolar mapping catheter, the anatomic acquisition is obtained by sequentially moving the mapping catheter, while the ablation catheter is parked in the mitral annulus. Two different views are shown (posterior and superior).
video 4 - CARTO-guided 3D images of RF delivery (pink and red dots) placed around the left PVs. The ablation catheter provides contact-force information, the arrow showing the force vector, and on top-left, the number of grams quantifying the tissue contact. Ablation lesions covering the full circumference around the left PVs are shown.
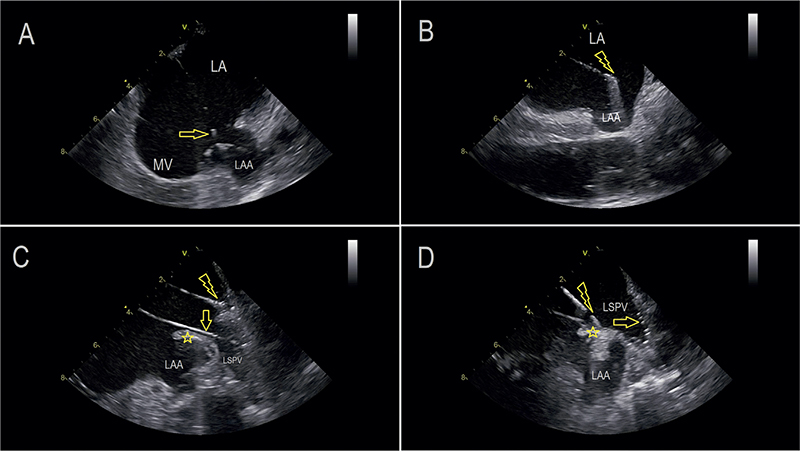
Figure 2 – ICE imaging sequence examples of LA mapping and ablation. These were recorded after the ICE catheter was placed in the LA cavity across the septum. A) A multipolar high-density mapping catheter (Pentarray – Biosense Webster, marked by arrow) is collecting anatomic and electric data around the left atrial appendage (LAA). MV – mitral valve. B) The tip of the contact force-sensor ablation catheter is floating in the LA cavity. As it is not touching any structure, this is a good spot to calibrate the sensor as zero force. This step is needed before initiating RF delivery. C) The ablation catheter is highlighted at the roof of the LA around the LSPV. The mapping catheter (arrow) is inside the LSPV monitoring its electrical connection to the LA. It is clear that the ablation catheter is in the PV antrum and not delivering energy inside the vein. D) Ablation in the ridge (*) between the LSPV and the LAA. The mapping catheter is inside the LSPV (arrow).
Abstract
Background: The use of ionizing radiation in medical procedures is associated with significant health risks for patients and the health care team.
Objectives: Evaluate the safety and acute efficacy of ablation for atrial fibrillation (AF) and supraventricular arrhythmias (SVTs) using an exclusively non-fluoroscopic approach guided by intracardiac echo (ICE) and 3D-mapping.
Methods: 95 pts (mean age 60 ± 18 years, 61% male) scheduled for AF Ablation (69 pts, 45 paroxysmal AF and 24 persistent AF) or non-AF SVT (26 pts – 14 AV node reentry, 6 WPW, 5 right atrial (RA) flutters, 1 atrial tachycardia) underwent zero fluoro procedures. Nine patients (9.5%) had permanent pacemakers or defibrillator resynchronization (CRT-D) devices. Both CARTO (65%) and NAVx (35%) mapping systems were used, as well as Acunav and ViewFlex ICE catheters.
Results: Pulmonary vein isolation (PVI), as well as all other targets that needed ablation in both atria were reached and adequately visualized. No pericardial effusions, thrombotic complications or other difficulties were seen in these series. Difficult transseptal puncture (19 patients - 20%) was managed without fluoroscopy in all cases. No backup fluoroscopy was used, and no lead apparel was needed. Pacemaker interrogations after the procedure did not show any lead damage, dislocation, or threshold changes.
Conclusions: A radiation-free (fluoroless) catheter ablation strategy for AF and other atrial arrhythmias is acutely safe and effective when guided by adequate ICE and 3D-mapping utilization. Multiple different bi-atrial sites were reached and adequately ablated without the need for backup fluoroscopy. No complications were seen. (Arq Bras Cardiol. 2020; 114(6):1015-1026)
Keywords: Arrhythmias, Cardiac; Atrial, Fibrillation; Catheter Ablation; Fluoroscopy; radiation; Efficacy; Safety.