Volume 114, Nº 3, March 2020
DOI: https://doi.org/10.36660/abc.20190050X
ORIGINAL ARTICLE
Analysis of Risk Scores to Predict Mortality in Patients Undergoing Cardiac Surgery for Endocarditis
Fernando Pivatto Júnior
Clarissa Carmona de Azevedo Bellagamba
Eduardo Gatti Pianca
Fernando Schmidt Fernandes
Maurício Butzke
Stefano Boemler Busato
Miguel Gus
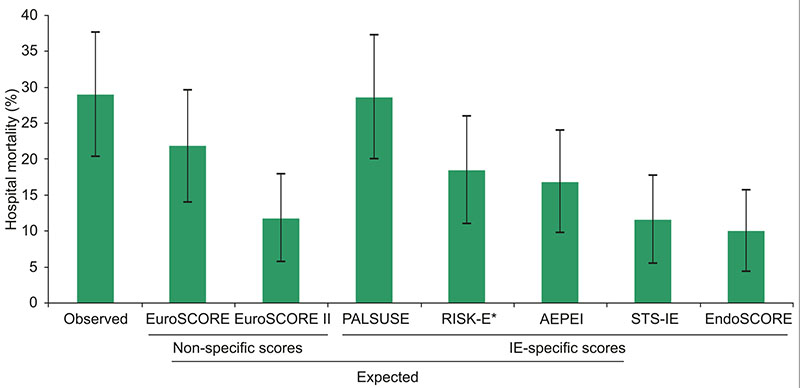
Figure 1 – Observed and expected hospital mortality according scores. *Observed mortality was 29.0%, except for the RISK-E score, which was 28.4% (5 right-sided infective endocarditis cases were excluded, since they are not included in this score analysis). Error bars represent 95% confidence intervals.
Abstract
Background: Risk scores are available for use in daily clinical practice, but knowing which one to choose is still fraught with uncertainty.
Objectives: To assess the logistic EuroSCORE, EuroSCORE II, and the infective endocarditis (IE)-specific scores STS-IE, PALSUSE, AEPEI, EndoSCORE and RISK-E, as predictors of hospital mortality in patients undergoing cardiac surgery for active IE at a tertiary teaching hospital in Southern Brazil.
Methods: Retrospective cohort study including all patients aged ≥ 18 years who underwent cardiac surgery for active IE at the study facility from 2007-2016. The scores were assessed by calibration evaluation (observed/expected [O/E] mortality ratio) and discrimination (area under the ROC curve [AUC]). Comparison of AUC was performed by the DeLong test. A p < 0.05 was considered statistically significant.
Results: A total of 107 patients were included. Overall hospital mortality was 29.0% (95%CI: 20.4-37.6%). The best O/E mortality ratio was achieved by the PALSUSE score (1.01, 95%CI: 0.70-1.42), followed by the logistic EuroSCORE (1.3, 95%CI: 0.92-1.87). The logistic EuroSCORE had the highest discriminatory power (AUC 0.77), which was significantly superior to EuroSCORE II (p = 0.03), STS-IE (p = 0.03), PALSUSE (p = 0.03), AEPEI (p = 0.03), and RISK-E (p = 0.02).
Conclusions: Despite the availability of recent IE-specific scores, and considering the trade-off between the indexes, the logistic EuroSCORE seemed to be the best predictor of mortality risk in our cohort, taking calibration (O/E mortality ratio: 1.3) and discrimination (AUC 0.77) into account. Local validation of IE-specific scores is needed to better assess preoperative surgical risk. (Arq Bras Cardiol. 2020; 114(3):518-524)
Keywords: Cardiovascular Surgical Procedures/mortality; Endocarditis/complications; Hospital Mortality; Risk Assessment.