Volume 112, Nº 2, February 2019
DOI: http://www.dx.doi.org/10.5935/abc.20180251
ORIGINAL ARTICLE
Long Term Cardiovascular Outcome Based on Aspirin and Clopidogrel Responsiveness Status in Young ST‑Elevated Myocardial Infarction Patients
Mustafa Umut Somuncu
Ali Riza Demir
Seda Tukenmez Karakurt
Huseyin Karakurt
Turgut Karabag
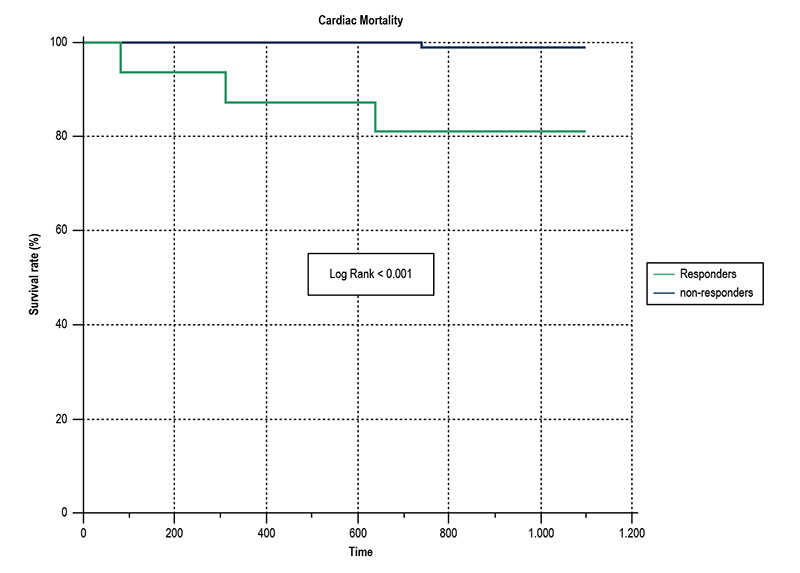
Figure 2 – Kaplan-Meier analysis showing 3-year cardiac mortality rate according to antiplatelet response. Patients with adequate response to aspirin and/or clopidogrel were considered “responders”. Patients with both aspirin and clopidogrel resistance were considered non-responders.
Abstract
Background: A subset of patients who take antiplatelet therapy continues to have recurrent cardiovascular events which may be due to antiplatelet resistance. The effect of low response to aspirin or clopidogrel on prognosis was examined in different patient populations.
Objective: We aimed to investigate the prevalence of poor response to dual antiplatelet therapy and its relationship with major adverse cardiovascular events (MACE) in young patients with ST-elevation myocardial infarction (STEMI).
Methods: In our study, we included 123 patients under the age of 45 with STEMI who underwent primary percutaneous intervention. A screening procedure to determine both aspirin and clopidogrel responsiveness was performed on the fifth day of admission. We followed a 2x2 factorial design and patients were allocated to one of four groups, according to the presence of aspirin and/or clopidogrel resistance. Patients were followed for a three-year period. A p-value less than 0.05 was considered statistically significant.
Results: We identified 48% of resistance against one or more antiplatelet in young patients with STEMI. More MACE was observed in patients with poor response to dual platelet therapy or to clopidogrel compared those with adequate response to the dual therapy (OR: 1.875, 1.144‑3.073, p < 0.001; OR: 1.198, 0.957-1.499, p = 0.036, respectively). After adjustment for potential confounders, we found that poor responders to dual therapy had 3.3 times increased odds for three-year MACE than those with adequate response to the dual therapy.
Conclusion: Attention should be paid to dual antiplatelet therapy in terms of increased risk for cardiovascular adverse events especially in young patients with STEMI. (Arq Bras Cardiol. 2019; 112(2):138-146)
Keywords: Acute Coronary Syndrome; Aspirin/adverse effects; Platelet Aggregation; Young Adult; ST Elevation Myocardial Infarction; Mortality.