Volume 111, Nº 6, December 2018
DOI: http://www.dx.doi.org/10.5935/abc.20180181
ORIGINAL ARTICLE
Paroxysmal Atrial Fibrillation Catheter Ablation Outcome Depends on Pulmonary Veins Anatomy
Gabriel Odozynski
Alexander Romeno Janner Dal Forno
Andrei Lewandowski
Hélcio Garcia Nascimento
André d’Avila
Dr. Gabriel Odozynski
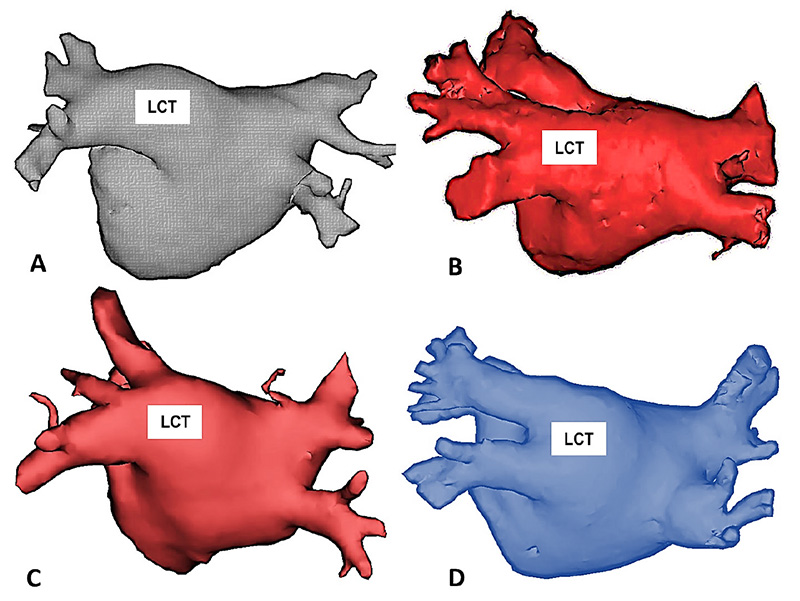
Figure 2 – Examples of patients with Common Trunk of the Left Pulmonary Veins (LCT) obtained from Computed Tomography performed before the catheter ablation procedure. In all cases, the left pulmonary veins coalesce before insertion into the left atrium and the minimum distance between the common ostium and the beginning of the bifurcation between the lower and upper branches of the common trunk is 10 mm. All the examples are in the posterior-anterior projection highlighting the posterior wall of the left atrium.
Abstract
Background: Pulmonary veins (PV) are often the trigger to atrial fibrillation (AF). Occasionally, left PVs converge on a common trunk (LCT) providing a simpler structure for catheter ablation.
Objective: To compare the clinical characteristics and outcomes of ablation in paroxysmal atrial fibrillation (PAF) of patients with or without LCT.
Methods: Case-control study of patients undergoing first-ever catheter ablation procedure for drug refractory PAF. The information was taken from patients’ records by means of a digital collection instrument, and indexed to an online database (Syscardio®). Clinical characteristics and procedures were compared between patients with or without LCT (LCT x n-LCT), adopting a level of statistical significance of 5%. The primary endpoint associated with efficacy was lack of atrial arrhythmia over the follow-up time.
Results: One hundred and seventy two patients with PAF were included in the study, 30 (17%) LCT and 142 (83%) n-LCT. The clinical characteristics, comorbidities, symptoms scale and risk scores did not differ between the groups. There was AF recurrence in 27% of PAF patients in the n-LCT group and only 10% of patients in the LCT group (OR: 3.4 p: 0.04) after a follow-up of 34 ± 17 months and 26 ± 15 months respectively.
Conclusion: Patients with a LCT have a significantly lower recurrence rate when compared to patients without this structure. It is mandatory to report the results of AF catheter ablation as a PV anatomical variation function. (Arq Bras Cardiol. 2018; 111(6):824-830)
Keywords: Atrial Fibrillation/physiopathology; Arrhythmias, Cardiac; Catheter Ablation; Pulmonary Veins/physiopathology; Electrophysiologic Techniques, Cardiac.