Volume 111, Nº 2, August 2018
DOI: http://www.dx.doi.org/10.5935/abc.20180119
ORIGINAL ARTICLE
Persistent Inflammatory Activity in Blood Cells and Artery Tissue from Patients with Previous Bare Metal Stent
Pedro Silvio Farsky
Mario H. Hirata
Renato Tambellini Arnoni
Antonio Flavio Sanches Almeida
Mario Issa
Paula Helena Ortiz Lima
Maria de Lourdes Higuchi
Hui T Lin-Wang
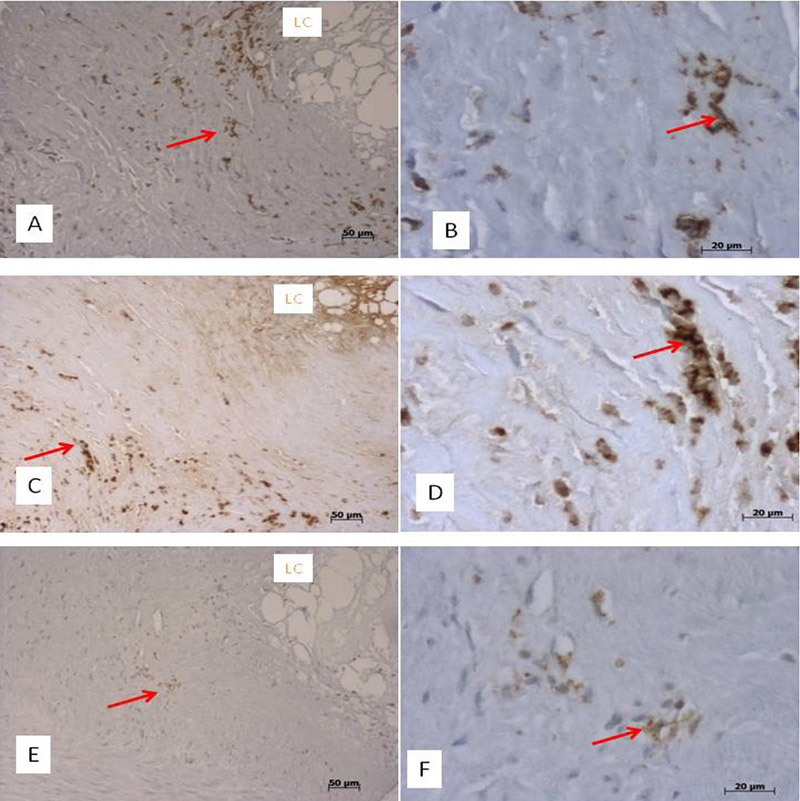
Figure 3 – Panoramic (left side) and high-power view (right side) of immunostained arterial intima-media layer from individuals with previous stent implantation. Panels A and B show MHCII-positive cells, with morphology of macrophages (arrows), surrounding the lipid core (LC). Panels C and D show a large amount of TNF-alpha in the cytoplasm of inflammatory cells (arrows) and in the lipid core (LC). Panels E and F exhibit fewer inflammatory cells positive for IL-6 protein in similar sites (arrows).
Abstract
Background: Studies have pointed out a higher mortality after coronary artery bypass surgery (CABG) in patients with stent.
Objective: To evaluate inflammatory markers in peripheral blood cells and in coronary artery tissue samples obtained during CABG in patients with stent compared to controls.
Methods: The case series consisted of two groups, one with previous stent implantation (n = 41) and one control (n = 26). The expression of the LIGHT, IL-6, ICAM, VCAM, CD40, NFKB, TNF, IFNG genes was analyzed in peripheral blood cells collected preoperatively. The coronary artery was evaluated for: interleukin-6, ICAM, VCAM, CD40, NFKB, TNF-alpha and IFN-gamma by immunohistochemistry. A total of 176 tissue samples were grouped for analysis in: A1- arteries with stent (n = 38); A2- native arteries from patients with stent in another artery (n = 68); and A3- arteries without stent from controls undergoing routinely CABG surgery (n = 70). A significance level of 0.05 was adopted.
Results: Patients with stent showed higher TNF (p = 0.03) and lower CD40 gene expression (p = 0.01) in peripheral blood cells than controls without stent. In coronary artery samples, the TNF-alpha protein staining was higher in the group A1, not only in the intima-media layer (5.16 ± 5.05 vs 1.90 ± 2.27; p = 0.02), but also in the adipose tissue (6.69 ± 3.87 vs 2.27 ± 4.00; p < 0.001). Furthermore, group A1 had a higher interleukin-6 protein staining in adipose tissue than group A3 (p = 0.04).
Conclusion: We observed a persistently higher systemic TNF expression associated with exacerbated TNF-alpha and interleukin-6 local production in patients with stents. This finding may contribute to a worse clinical outcome. (Arq Bras Cardiol. 2018; 111(2):134-141)
Keywords: Percutaneous Coronary Intervention; Blood Cells; Inflammation; Stents; Polymerase Chain Reaction; Immunohistochemistry; Tumor Necrosis Factor-alpha; Interleukin-6.