Volume 110, Nº 2, February 2018
DOI: http://www.dx.doi.org/10.5935/abc.20180006
ORIGINAL ARTICLE
Autonomic and Vascular Control in Prehypertensive Subjects with a Family History of Arterial Hypertension
Josária Ferraz Amaral
Diana de Medeiros Andrade Borsato
Isabelle Magalhães Guedes Freitas
Edgar Toschi-Dias
Daniel Godoy Martinez
Mateus Camaroti Laterza
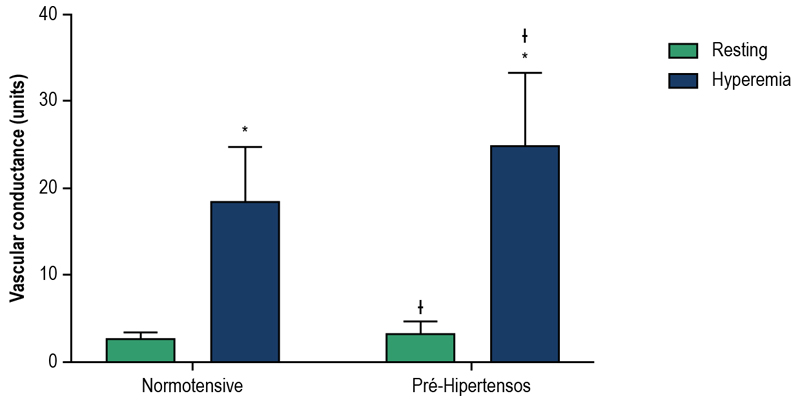
Figure 1 – Vascular function. Data represented as mean ± standard deviation; ANOVA of two factors for repeated measures: *: significant differences in relation to rest; ᵻ: significant differences in relation to the normotensive group.
Abstract
Background: Individuals with a family history of systemic arterial hypertension (FHSAH) and / or prehypertension have a higher risk of developing this pathology.
Objective: To evaluate the autonomic and vascular functions of prehypertensive patients with FHSAH.
Methods: Twenty-five young volunteers with FHSAH, 14 normotensive and 11 prehypertensive subjects were submitted to vascular function evaluation by forearm vascular conductance (VC) during resting and reactive hyperemia (Hokanson®) and cardiac and peripheral autonomic modulation, quantified, respectively, by spectral analysis of heart rate (ECG) and systolic blood pressure (SBP) (FinometerPRO®). The transfer function analysis was used to measure the gain and response time of baroreflex. The statistical significance adopted was p ≤ 0.05.
Results: Pre-hypertensive individuals, in relation to normotensive individuals, have higher VC both at rest (3.48 ± 1.26 vs. 2.67 ± 0.72 units, p = 0.05) and peak reactive hyperemia (25, 02 ± 8.18 vs. 18.66 ± 6.07 units, p = 0.04). The indices of cardiac autonomic modulation were similar between the groups. However, in the peripheral autonomic modulation, greater variability was observed in prehypertensive patients compared to normotensive individuals (9.4 [4.9-12.7] vs. 18.3 [14.8 26.7] mmHg2; p < 0.01) and higher spectral components of very low (6.9 [2.0-11.1] vs. 13.5 [10.7-22.4] mmHg2, p = 0.01) and low frequencies (1.7 [1.0-3.0] vs. 3.0 [2.0-4.0] mmHg2, p = 0.04) of SBP. Additionally, we observed a lower gain of baroreflex control in prehypertensive patients compared to normotensive patients (12.16 ± 4.18 vs. 18.23 ± 7.11 ms/mmHg, p = 0.03), but similar delay time (-1.55 ± 0.66 vs. -1.58 ± 0.72 s, p = 0.90).
Conclusion: Prehypertensive patients with FHSAH have autonomic dysfunction and increased vascular conductance when compared to normotensive patients with the same risk factor. (Arq Bras Cardiol. 2018; 110(2):166-174)
Keywords: Hypertension / genetic; Autonomic Nervous System; Risk Factors; Endothelium, Vascular / physiopathology.