Volume 115, Nº 2, August 2020
DOI: https://doi.org/10.36660/abc.20180346
ORIGINAL ARTICLE
Complete Revascularization Versus Treatment of the Culprit ArteryOnly in ST Elevation Myocardial Infarction: A Multicenter Registry
Julia Cremona Cadore
Mariana Vargas Furtado
Rogério Tumelero
Alexandre Tognon
Ana Maria Krepsky
Denis Cadore
Karen Brasil Ruschel
Julia Caldas Bedin
Thais Conte
Carisi Anne Polanczyk
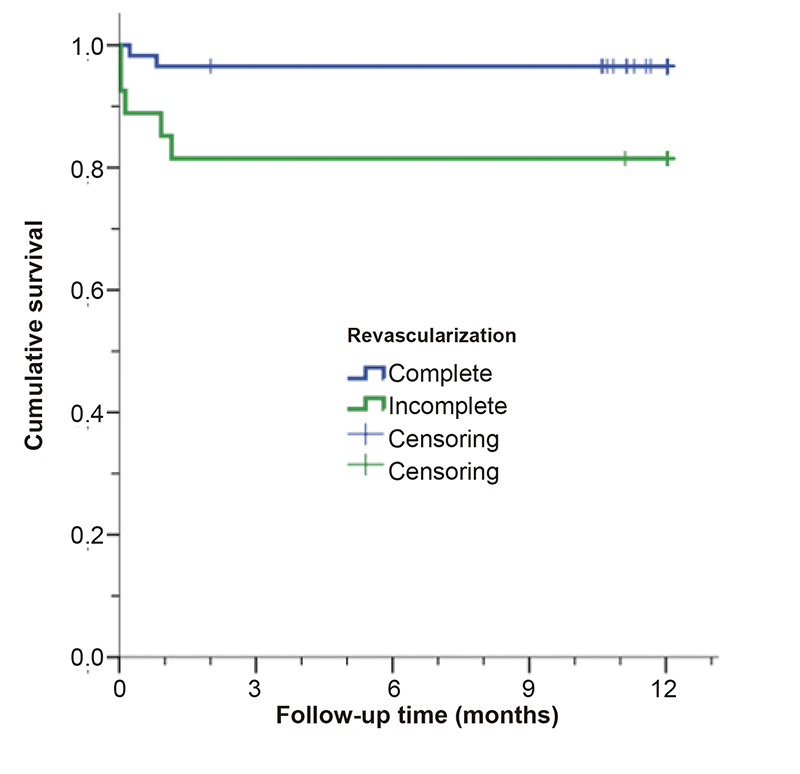
Figure 1 – Twelve-month survival after complete revascularization (CR) and incomplete revascularization (IR) in patients with acute ST-segment elevation myocardial infarction (STEMI) and multivessel disease. *Log-rank test.
Abstract
Background: Data on the management and prognosis of patients with ST-segment elevation myocardial infarction (STEMI) and multivessel disease are limited in Brazil, showing that the available revascularization strategies should be investigated.
Objective: To assess the outcomes of complete revascularization versus treatment of the culprit artery only in patients with STEMI and multivessel disease.
Methods: A prospective cohort study was conducted at two medical centers in southern Brazil with a 1-year follow-up after the index procedure. The primary outcome was a composite of cardiac death, reinfarction, or recurrent angina, while the secondary outcome was stroke, nonfatal cardiac arrest, major bleeding, or need for reintervention. The probability of outcomes occurring was compared between the groups using binary logistic regression. A p-value < 0.05 was considered statistically significant.
Results: Eighty-five patients were included. Their mean age was 62±12 years, and 61 (71.8%) were male. Fifty-eight (68.2%) were treated with complete revascularization and 27 (31.8%) with incomplete revascularization. The chance of both the primary and secondary outcomes occurring was significantly greater among patients treated with incomplete revascularization when compared to those treated with complete revascularization (odds ratio [OR] 5.1, 95% confidence interval [CI] 1.6-16.1 vs. OR 5.2, 95% CI 1.2-22.9, respectively), as well as cardiac death (OR 6.4, 95% CI 1.2-35.3).
Conclusion: Registry data from two centers in southern Brazil demonstrate that the complete revascularization strategy is associated with a significant reduction in primary and secondary outcomes in a 1-year follow-up when compared to the incomplete revascularization strategy (Arq Bras Cardiol. 2020; 115(2):229-237)
Keywords: ST Elevation Myocardial Infarction/mortality, Cohort Studies; Hemodynamic; Death Certificates; Angina Pectoris; Stroke; Heart Arrest; Death Certificates; Angina Pectoris; Stroke; Heart Arrest; Percutaneous Coronary Interventions.